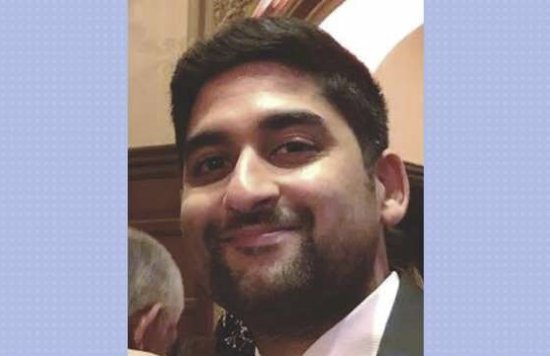
Viral Kantaria is the Trust’s new Programme Director for Community Mental Health Transformation. He joins ELFT from NHS England where he worked on the NHS Long Term Plan. In this interview he tells us about his career path, his ambition to make mental health care truly serve local people, who his heroes are (his mum) and how he relaxes.
Tell us about your career background? How did you come to be in this field?
I came into healthcare about 10 years ago. I worked for a couple of ministers in the Coalition Government: the Rt Hon. Paul Burstow and then the Rt Hon. Sir Norman Lamb. My job was to support the wide range of portfolio areas of both– including mental health. It was a civil service non-political role. They were passionate advocates for mental health.
Sir Norman had specific lived experience himself within his own family, and he very much made a mission within government to radically improve mental health care – that rubbed off on me.
I was involved with policy initiatives around things like children and young people’s mental health, suicide prevention and the Mental Health Crisis Care Concordat launched in 2014, which laid the foundation for all of the improvements that we've seen in crisis care ever since – but we still have a way to go!
This ignited my passion for mental health. I then moved to a policy role at the Department of Health, leading on mental health crisis care policy and legislation relating to the Mental Health Act, with particular focus on policing - working to develop new legislation to radically reduce use of police cells as a place of safety.
Did you start off with this type of career in mind?
I studied English Literature and Spanish at University, then a Master's in Modern English Literature. So not health-related at all! I was considering a PhD and a life in academia but no field had particular appeal. But public service did!
It’s something that I feel really strongly about now. After a decade of having worked for Government, and now for the NHS, the ethos of service to the public is really important to me - trying to improve services and ultimately the lives of people up and down the country. And from now on, specifically the lives of people in East London, Bedfordshire and Luton.
What attracted you to this role? Why do you think it’s important to deliver such a transformative programme?
Two things: Firstly, ELFT has a brilliant reputation. You have a humility here which is unique, people are humble and there is a positive culture. I want to be part of something progressive, and in doing that to really push the boundaries and not be afraid of having very high levels of ambition for the people we serve.
I’ve been in roles shaping national policy. I thought: now is the time to be involved in making things happen on the ground and at micro level. I want to really understand the local story, local politics, what makes people tick and what works, to change things at a neighbourhood level. Having been involved in developing the NHS Long Term Plan for mental health, it feels right to be part of the implementation stage.
We’re at a critical juncture now in terms of moving forward. So getting this embedded as ‘business as usual’ will change what happens when someone needs mental health care and support. We can showcase the amazing work in East London to colleagues across our local system but also to colleagues across the rest of London and the country.
Have mental health issues touched you or someone close to you?
I'd be very surprised if anyone said they hadn’t. Most people will have some experience of mental health challenges at some point. I think many mental health issues manifest in a way that never really comes to the attention of the NHS. I've had a number of very close friends and work colleagues who have been affected by a range of mental health issues – such as sleep issues and insomnia, to varying levels of anxiety, and eating disorders. I have close friends who have complex emotional needs - others with a lifelong bipolar disorder diagnosis.
Within my family, I've seen the sort of traits that we might associate with mental health issues. I come from an Indian family and the way that mental health is perceived and discussed among Indian communities is different. I think it’s interesting to think about the way we ‘receive’ experiences in our personal lives and what is shown to the outside world.
We've made a lot of progress around talking more comfortably around things like anxiety and depression - how you would say - the milder end of common mental health problems. What we haven't really done is started to talk about more severe mental health problems in the same way. But I feel there is a momentum that's unstoppable at this point, and I really hope that programmes like the Community Mental Health Transformation programme can start to bring some of that out a bit more clearly – to make us feel more comfortable to talk about sometimes really debilitating mental health difficulties in day-to-day life and language.
What do you think the challenges will be?
I think one of the biggest challenges for me is the context in which we're trying to do this. We're still in the middle of a global pandemic here, so I am reflecting on the fact that not only are our staff exhausted physically, they are also mentally and emotionally depleted.
I think also of our local communities, patients, carers and families out there, who are all facing their own kind of individual or mini collective challenges. Many would have had a significant need for some form of care, support and treatment beforehand. But what's happened is likely to have affected the severity of people’s needs, the acuity, and the complexity.
I think we need to take this into account when trying to implement change and empower our local teams. The ELFT transformation programme doesn’t at all have a ‘top-down’ culture, but it requires people to have energy and the will to do things differently. How can we use all of that to re-energise people so that the Community Mental Health Transformation programme is seen as a positive, optimistic initiative that brings hope to people? And I don’t mean glossing over the difficulties because, a lot of the reason we want to make changes is because we know things aren’t working. We know that we can do things better. It's actually the system that's not allowing us to do that. And that's what we need to change.
The good things that we've achieved to date and our level of ambition need to continue to allow us to fulfil our future vision and consolidate our gains. Our patients and carers need hope and optimism. So I think building and continuing to push is a big challenge.
I think another one is the longstanding inequalities that a lot of our communities and patient groups have faced. COVID has highlighted this in a really quite harrowing way, with some of the highest death rates, if not the highest death rates in the country, particularly in Hackney and Newham. I am aware a huge amount of work is already underway around things like the Patient and Carer's Race Equality Framework and specific work tackling inequalities for people with severe mental health problems. It’s two sides of the same coin and we must address this in our transformation work.
The sheer amount of work that we still have to do to make this happen is another kind of challenge. But the kind of commitment that I've seen in the passion from people here makes me think - absolutely anything is possible!
What will your first steps be?
I've managed to get my laptop more or less 100% sorted (thanks Anabel [Ferras]!). I've started my induction meetings with key colleagues across the Trust and that's going to carry on for several weeks. I'm really keen to meet our incredible local partners too. I really want to understand what's happening in our local Voluntary & Community Sector and meet the leaders. This will give me a clear bird’s eye view of where we're at with the transformation work. It will help us to consider whether we need to reset our priorities, whether there are areas that are more neglected than others - that sort of thing.
What difference has the programme made so far, or is likely to make in the long term. And if you time travelled three years, what would services look like in 2024?
A lot has already happened in East London. It may not yet be fully quantifiable at patient level, but the foundations are in place. The enthusiasm and engagement levels of staff working on this transformation is palpable as they move into ‘business as usual’ blended team roles.
For someone coming into this role to be able to work with that level of commitment and energy is just a dream really. Obviously, I also want to understand what data we are collecting around patient care to quantify the hopefully positive impact the changes are creating.
I'd also like to see some of the narrative and qualitative information from service users and carers because it's not just about numbers on spreadsheets; at the end of the day, do patients think that this change is working for them and is it delivering what they want and need? If not, then we need to learn and change. The People Participation Leads and Workers I’ve listened to have been brilliant at articulating how we need to co-produce from design to delivery and pursue what are actually often pretty obvious logical goals about our new care offer.
I want us to be able to do two things: one is to significantly improve timely access to care, to stop saying “No” to people, and to radically reduce some of the long waiting times for people who are in need of specific packages of care. For example, a course of psychological therapy for a severe mental health problem.
Secondly, to radically improve the quality of care that people receive so that it is meaningful intervention-based care. So not having service users spending a lot of their time sitting inactively on team caseloads – but for there to be many interventions from different community resources addressing the issues that cause or keep people mentally unwell, and for more people with lived experience to be part of our MDTs, paid fairly, with supervision and career development, and influencing our strategic planning.
In three years’ time, I'd want things to be totally different – to be really thinking about population health on a place-based basis, if that makes sense. We need to think about what we can offer people with lower levels of complexity, as well as to people with the highest levels of complex needs within a local community. I'd want us to be moving away from thinking about dusty outpatient clinics to care genuinely delivered within the community – where people live, on the high street and in community spaces.
In three years’ time, I'd want us to be talking about how we have actually made inroads into the current overrepresentation of people from certain ethnic minority backgrounds among the detained inpatient population, because we've actually proactively understood their needs much earlier. And because we've managed to address their needs by working co-productively with them, their carers’ and with the communities in which they live.
I want us to be working in partnership, for example, by funding local grassroots organisations to provide support interventions as part of a kind of integrated offer so that we're not seeing people contacting or coming into contact with services at crisis point or via the criminal justice system because of a missed opportunity. Our services should be proactive, preventative, flexible services where we were actually saying “Yes, we can help you” to people as early as possible. They shouldn’t have to batter the door down, and people with long term severe mental health problems should feel safe to say when they aren’t feeling right at a much earlier stage. People’s needs change and our services ought to be able to respond accordingly.
What did you want to be when you were growing up?
I didn't really know to be honest. I mean, there were a few things that kind of knocked around. My mother wanted me to be a lawyer! I thought that sounded great until I thought the reality would be very intense. At one point I wanted to become a literary translator, having studied Spanish at university.
My family background will be very familiar to anyone who knows about Indian families - that you're expected to do one of a small range of things such as law, medicine, pharmacy or accountancy. I was always quite open-minded about what I wanted to do and my family now know that healthcare and mental health is where I am at! There's still so much more to do, and within my lifetime, I'm hoping I can kind of push things forward so that the injustice and disparity feels like a thing of the past.
So what do you do to relax and unwind?
I think my answer would have been a lot different a year ago than it is now. I think all our options are quite limited at the moment, so to relax and unwind I can do two extremes. I can settle down in front of The West Wing which I'm catching up on at the moment, or go for a run. Running is probably one of the things that has really helped me over the past year in terms of clearing my head.
What or who has been the greatest influence on your life, would you say?
I think probably my mum in all honesty. She came to this country as a refugee in the 70s following Idi Amin’s expulsion of Asians from Uganda. I was vaguely aware of her story growing up, but not really. One day for an English project at school, the teacher set a task to interview a member of your family about their childhood and that's the first time that I heard the full story. It was a pretty traumatic story of being forced out of the country of her birth and happy childhood at gunpoint.
My mum's made a lot of sacrifices for us. Her studies were totally disrupted by being expelled from Uganda. She was very much a career woman until marriage. She did the classic thing and gave up her career to take care of the family. But her time came again – she studied from scratch and got two degrees once my sisters and I had all hit double digits in age.
She used to get up at 5am! There were 12 of us living in a big house for quite a few years but she made it all tick. I have no idea how she did that. My mum is a influence on my life. It’s been hard not seeing her this year.
Three things on you bucket list.
All short term: I definitely want to do a skydive at some point. I would really like to go back to South America having been there once on holiday in 2013. It would be good to practice my Spanish and learn some new dialects and meet new people and learn some more history. It's a totally fascinating place.
I’d also like to improve my French. My conversational French isn’t bad but my written skills leave a lot to be desired at the moment!
What would your alternative career be if you weren’t in the NHS?
I think I'd be a writer. Actually, I did like writing when I was younger, but I never really thought that that was a career option and it never really felt like a realistic option. So a writer, novelist or poet maybe.
Quick fire questions:
Tea or coffee? Neither…
Crossword or Sudoku? Crossword.
Book or Netflix? Uh, I'd like to say book, but the truth is probably Netflix.
Dessert or cheeseboard? Uh dessert, but my French girlfriend would not be happy (she’d say both).
If you were a pet owner, a cat or a dog? Cat.
And London or Paris? I think we've already had the answer to this.
Oh wow, yeah I'm gonna go London – just to be contrary.